Table of Contents
ToggleWhite patches in the mouth can be as alarming as finding a sock in the dryer that doesn’t match. They can pop up unexpectedly and leave anyone scratching their head. What are these mysterious spots? Are they a sign of a secret alien invasion or just a case of too much pizza? Spoiler alert: it’s usually the latter.
Overview of White Patches in Mouth
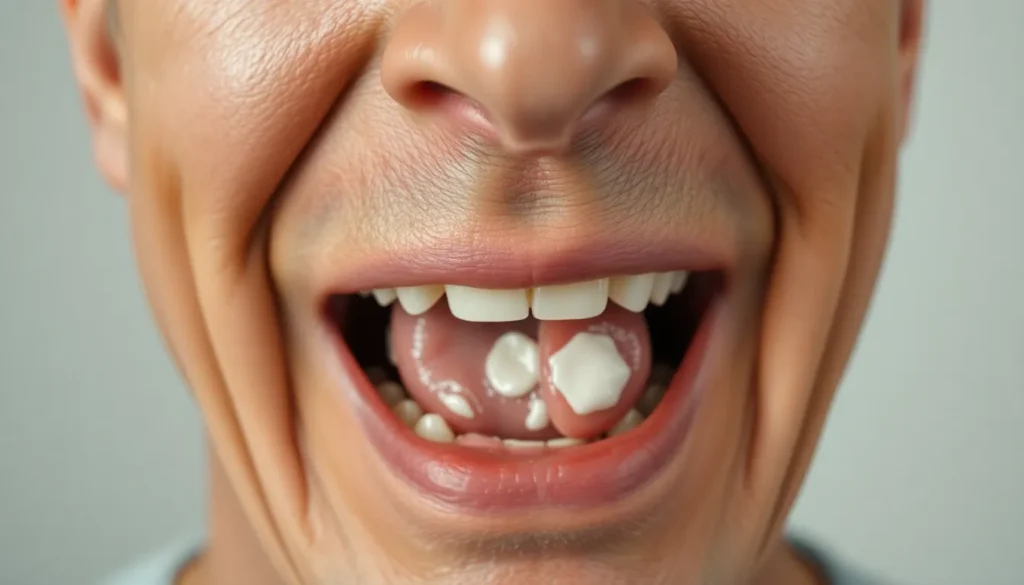
White patches in the mouth can indicate various conditions. These lesions may appear on the cheeks, gums, tongue, or roof of the mouth. Several causes, such as infections, irritations, or underlying health issues, contribute to their formation.
Oral thrush, a fungal infection caused by Candida yeast, often produces white lesions. Symptoms include pain or discomfort in the mouth. Geographic tongue, characterized by irregular patches, can also create a white appearance on the tongue’s surface.
Lichen planus could present as white streaks and patches in the mouth. This condition involves an inflammatory response affecting mucous membranes. Allergic reactions to medications or dental products sometimes lead to white patches as well.
Additionally, smoking or chewing tobacco causes leukoplakia, which manifests as thick, white patches. This condition requires a healthcare professional’s attention due to its potential link to oral cancer.
Maintaining proper oral hygiene is crucial in preventing the development of white patches. Regular dental check-ups can help identify early signs of conditions associated with these lesions. Awareness of dietary choices may also play a significant role; acidic or spicy foods can irritate the mucous membranes, increasing the likelihood of patches forming.
If white patches persist or cause discomfort, consulting a healthcare professional is recommended. A definitive diagnosis usually requires an examination and possibly a biopsy of the patch to determine the exact cause.
Common Causes of White Patches

White patches in the mouth can arise from various conditions. Understanding their origins aids in seeking appropriate treatment.
Oral Thrush
Oral thrush represents a common fungal infection caused by Candida yeast. It causes white lesions on the tongue, cheeks, and sometimes the roof of the mouth. Individuals with compromised immune systems or those taking antibiotics often experience this condition. Symptoms include pain and difficulty swallowing. Treatment typically involves antifungal medications, which effectively alleviate the lesions.
Leukoplakia
Leukoplakia manifests as thick, white patches on the gums, tongue, or inside the cheeks. Tobacco use frequently causes this condition, with potential links to irritation from rough teeth or dental appliances. Although often harmless, leukoplakia can sometimes indicate pre-cancerous changes. Regular dental visits allow for monitoring and management. In some cases, a biopsy might be necessary to rule out cancers.
Lichen Planus
Lichen planus appears as white, lacy patches or lesions within the mouth. This inflammatory condition affects the mucous membranes and can also impact skin. Stress or certain medications trigger lichen planus in some individuals. While it may cause discomfort, it isn’t contagious. Management usually involves corticosteroids to reduce inflammation and pain. Regular check-ups assist in monitoring the condition effectively.
Diagnosis and Examination
Diagnosing white patches in the mouth relies on careful evaluation and specific tests. Various approaches are used to identify the underlying conditions.
Visual Inspection
During a visual inspection, a healthcare professional examines the mouth for distinct characteristics of white patches. They assess the location, size, and texture. Observations include whether patches are raised, flat, or lacy. Each of these factors offers clues to potential causes. For example, oral thrush typically appears as creamy white lesions, while leukoplakia presents as thick, white areas. Visual assessments play a critical role in determining the need for further tests.
Diagnostic Tests
Diagnostic tests may be necessary to confirm the origin of white patches in the mouth. Healthcare providers often recommend a biopsy to examine tissue samples microscopically. Blood tests can help diagnose infections or underlying systemic conditions contributing to the lesions. Additionally, fungal cultures might identify specific pathogens like Candida. Each test provides valuable information that aids in making an accurate diagnosis and developing an appropriate treatment plan.
Treatment Options
Various treatment options address white patches in the mouth, focusing on the specific cause of the condition. Healthcare professionals often recommend targeted approaches, such as medication or home remedies.
Medication
Antifungal medications treat oral thrush effectively. These typically include nystatin or fluconazole, which target fungal infections directly. Corticosteroids may alleviate inflammation associated with lichen planus. If leukoplakia is present, frequent monitoring and sometimes surgical removal might be necessary. Antibiotics can manage secondary infections if the patches lead to ulcers or lesions. Patients should always consult healthcare providers for appropriate dosages and treatment plans tailored to their needs.
Home Remedies
Certain home remedies provide relief for mild cases of white patches. Rinsing with salt water can reduce irritation and promote healing. Using baking soda mixed with water offers another soothing option, balancing oral pH levels. Additionally, maintaining proper hydration helps to keep the mouth moist, aiding recovery. A diet rich in fruits and vegetables supports overall oral health. Consulting a healthcare professional remains crucial, particularly if symptoms persist despite these remedies.
Importance of Medical Consultation
Seeking medical consultation for white patches in the mouth plays a crucial role in determining the underlying cause. Healthcare professionals evaluate symptoms and perform examinations to identify specific conditions like oral thrush or leukoplakia. Consulting a doctor ensures a thorough assessment, especially when patches persist or cause discomfort.
Visual inspections provide insights into the patches’ characteristics, allowing professionals to differentiate between potentially serious and benign conditions. Diagnostic tests, including biopsies or blood tests, are often necessary for precise identification. Engaging with a healthcare provider can lead to tailored treatment plans based on accurate diagnoses.
Recognizing potential warning signs prompts timely action. For example, patches that change color or size may indicate an evolving condition, signaling the need for immediate attention. Educating oneself about oral health emphasizes the importance of reporting unusual changes to a dentist or physician.
Regular dental check-ups contribute significantly to preventive care. Routine examinations can identify early signs of oral health issues before they escalate. White patches should never be ignored, as they may signify serious underlying problems.
Ultimately, trusting professional expertise leads to better health outcomes. A timely consultation not only alleviates concerns but also guides individuals toward effective management strategies. Investing in dental health through proactive measures ensures long-term well-being and peace of mind.
White patches in the mouth can be concerning but understanding their causes and implications is essential for effective management. Whether linked to infections or other conditions proper diagnosis plays a crucial role in determining the right treatment. Maintaining good oral hygiene and seeking regular dental check-ups can help prevent these issues.
If white patches persist or cause discomfort consulting a healthcare professional is vital. With timely intervention and appropriate care individuals can achieve better oral health and address any underlying conditions effectively. Staying informed and proactive is key to ensuring long-term well-being.